First Aid
Simple Steps for First Aid
1. Be Prepared:
Always have a first aid kit available in your home, car and recreational vehicles. Take a first aid class and know CPR.
2. Safety:
Always insure the area is safe and for your own personal safety. The hazard that injured the patient or other hazards may still be present.
3. Breathing:
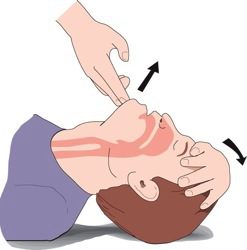
Clear Airway: Insure the patient is breathing if unconscious. If not gently tilt back the forehead to open mouth and airway. If breathing does not spontaneously return – perform rescue breathing if trained.

Choking: A person may be choking or have an airway blockage if he/she can’t speak, cough, or breathe while still conscious. Usually they will be holding their hands in the throat area. Do not give food or water. If breathing stops, for a child, turn him/ her upside down and smack hard between the shoulder blades three times. Check the mouth to see if the object can be removed. The best method for assisting an adult is the Heimlich maneuver which is a chest thrust performed just below the diaphragm.
4. Bleeding:

Stop any major bleeding. With your hand, apply direct pressure right over the wound, using a clean cloth, thick pad or bandage. Cold packs or ice may help with smaller cuts. Elevate the wound above the heart if possible. Apply bandage once the bleeding is under control.
Minor Cuts or Scrapes: Wash minor cuts, scratches, or scrapes with soap. Apply antiseptic and protect with a sterile bandage.
When does a wound need to be closed by your doctor (stitches) or an urgent care center?
- Wounds that are more than 0.25 in. (6.5 mm) deep, and that have jagged edges, or that gape open.
- Wounds longer than 0.75 in. (20 mm) that is deeper than 0.25 in. (6.5 mm).
- Deep wounds that go down to the fat, muscle, bone, or other deep structures.
- Deep wounds over a joint, especially if the wound opens when the joint is moved or if pulling the edges of the wound apart shows fat, muscle, bone, or joint structures.
- Wounds on the face, lips, eyelids or any area where you are worried about scarring (for cosmetic reasons).
- Wounds that continue to bleed after 15 minutes of direct pressure.
5. Circulation (Heart Beat):
Ensure proper circulation (a heartbeat present) if patient is unconscious – feel for carotid pulse at side of neck. If no pulse present – perform CPR immediately.

CPR can be performed by placing both hands in the center of the chest mid-sternum (between the nipples) and pushing hard and fast (2” depth with a rhythm of 100 compressions per minute). If an AED is available turn it on and follow the voice prompts for hook up and use.
6. Head injury:
Most common head injuries and bumps are minor and don’t require specialized attention or hospitalization. Even so minor injuries may cause persistent chronic symptoms, such as headache or difficulty concentrating, and you may need to call your doctor and take some time away from many normal activities to get enough rest to ensure complete recovery. However – If any of the following signs or symptoms are apparent, because they may indicate a more serious head injury Call 911 or go immediately to the hospital or your doctor if that may be quicker.
- Severe head or facial bleeding
- Bleeding or fluid leakage from the nose or ears
- Severe headache
- Change in level of consciousness for more than a few seconds
- Black-and-blue discoloration below the eyes or behind the ears
- Cessation of breathing
- Confusion
- Loss of balance
- Weakness or an inability to use an arm or leg
- Unequal pupil size
- Slurred speech
- Seizures
- Persistent crying
- Refusal to eat (infants)
- Bulging in the soft spot on the front of the head (infants)
- Repeated vomiting
7. Broken Bones/Dislocations:
Broken bones themselves – although very painful – are seldom life threatening. However they may be associated life threatening injuries such as severe bleeding or a head injury.
- Spinal and/or neck fractures are the most serious and if suspected don’t move the patient unless absolutely necessary for a life saving measure. Call 911.
- Major deformed broken bone and or dislocation. Stop any bleeding first. Then support with a splint (i.e. board, cardboard or rolled up newspaper, or a soft splint such as a pillow or rolled blanket). The splint should extend to the joint above and below the break. Secure the splint in place (i.e. bandages, duct tape, belt)
- Minor or unknown. Signs of a fracture are usually pain, swelling, unusual shape, or discolored skin. A visit to the doctor and an x-ray may be needed to confirm. Support the suspected injury and a cold pack may be used to help with pain and swelling.
Most broken bones by themselves and/or possible fractures are not critical life threatening emergencies so patient comfort and the safe and calm transportation to your doctor or urgent care is warranted.
8. Medical Emergencies:
Heart Attack
Some heart attacks are sudden and intense — the “movie heart attack,” where no one doubts what’s happening. But most heart attacks start slowly, with mild pain or discomfort. Often people affected aren’t sure what’s wrong and wait too long before getting help. Here are signs that can mean a heart attack is happening:
- Chest discomfort. Most heart attacks involve discomfort in the center of the chest that lasts more than a few minutes, or that goes away and comes back. It can feel like uncomfortable pressure, squeezing, fullness or pain.
- Discomfort in other areas of the upper body. Symptoms can include pain or discomfort in one or both arms, the back, neck, jaw or stomach.
- Shortness of breath with or without chest discomfort.
- Other signs may include breaking out in a cold sweat, nausea or lightheadedness. As with men, women’s most common heart attack symptom is chest pain or discomfort. But women are somewhat more likely than men to experience some of the other common symptoms, particularly shortness of breath, nausea, and back or jaw pain.
If you suspect a heart attack, take one small over-the-counter aspirin, Call 911 or go immediately to the hospital or your doctor if that may be quicker.
Stroke
Not all these signs occur in every stroke however usually in some combination. Sometimes they go away and return. Today stroke victims can benefit from new medications and treatments unavailable to patients in years past. But to be effective, these drugs must be given relatively quickly after stroke symptoms first appear. If you suspect a stroke, Call 911 or go immediately to the hospital or your doctor if that may be quicker.
- Face Drooping Does one side of the face droop or is it numb? Ask the person to smile.
- Arm Weakness Is one arm weak or numb? Ask the person to raise both arms. Does one arm drift downward?
- Speech Difficulty Is speech slurred, are they unable to speak, or are they hard to understand? Ask the person to repeat a simple sentence, like “the sky is blue.” Is the sentence repeated correctly?
- Sudden numbness or weakness of the leg
- Sudden confusion or trouble understanding
- Sudden trouble seeing in one or both eyes
- Sudden trouble walking, dizziness, loss of balance or coordination
- Sudden severe headache with no known cause
Insect Stings and Bites
Most insect bites and stings are more discomfort than danger, although can be painful, fortunately are not an emergency. Remove the insect stinger if present. Apply a cold pack. Take an over the counter antihistamine such as diphenhydramine (Benadryl) or a non-sedating one such as loratadine (Claritin) if concerned about any allergic reaction. If patient is already known to be seriously allergic they often have and carry an epi-pen. Follow the directions and help administer if needed. If whole body hives (rash) appear or difficulty breathing or major swelling (beyond the sting area) develops – call 911 or go immediately to the hospital or your doctor.
Poisoning
Any non-food substance swallowed by a child should be considered an immediate danger. Call the Poison Control Center at 800-222-1222. You should keep this number at each phone and saved on your cell phone. If possible, have the substance container on hand and try to determine how much was ingested. Follow the Poison Control Center directions.
General Illness
General illness is best resolved normally with rest, fluids and by consulting your primary care provider.
If loss of consciousness, seizures and/ or severe pain occurs that that is a cause for immediate care. Call 911 or go immediately to the hospital or your doctor.
Nausea and Vomiting
Usually, vomiting is generally harmless – and not an emergency by itself– although generally not pleasant at all – and often a result of motion sickness or “seasickness”, vertigo, early stages of pregnancy, a reaction to medication, emotional stress, reaction to smell or orders, food poisoning, stomach flu, and overeating. However it can sometimes be related to a more serious illness.
Call your doctor about nausea and vomiting:
- If the nausea lasts for more than a few days,
- If there is a possibility of being pregnant,
- If home treatment is not working, dehydration is present,
- A known injury (such as head injury or infection) has occurred recently,
- If vomiting occurs for more than one day, diarrhea and vomiting last more than 24 hours, or there are signs of dehydration,
- Take an infant or child under six years of age to the doctor if vomiting lasts more than a few hours, diarrhea is present, signs of dehydration occur, there is a fever, or if the child hasn’t urinated for 4-6 hours,
- Take a child over age six years of age to the doctor if vomiting lasts one day, diarrhea combined with vomiting lasts for more than 24 hours, there are any signs of dehydration, there is a fever higher than 101 degrees, or the child hasn’t urinated for six hours.
You should go seek immediate medical care if any of the following situations occur with vomiting:
- There is blood in the vomit (bright red or “coffee grounds” in appearance)
- Severe headache or stiff neck
- Lethargy, confusion, or a decreased alertness
- Severe abdominal pain
- Diarrhea
- Rapid breathing or pulse
Vial of Life Program
The La Pine Lions Club in conjunction with the La Pine Rural Fire Protection District is proud to announce the implementation of the Vial Of Life program. The Vial Of Life is used in the event you are incapacitated or have a life threatening emergency that renders you or a loved one unable to communicate to medical personnel. The Vial will provide a means to supply medical personnel vital information about your medical conditions and medications to aid in your emergency treatment. The Vial Of Life is a free resource to the residents of the La Pine Rural Fire Protection District. Funding for the program is 100% funded by donations. A Vial can be obtained from your local La Pine Fire Station, or can be obtained at local events scheduled in the future with in the district. Click here to print the form.
For more information or to become a donating member of the community, contact Brett Hulstrom.
